Introduction
Exercise is critical for the effective prevention and treatment of type 2 diabetes, but compliance with an active lifestyle that includes regular moderate-to-vigorous physical activity is low in the general adult population in Europe and the United States. Compliance is even lower in people who have been diagnosed with type 2 diabetes or in adults who are at risk of developing the disease. Sedentary behavior, on the other hand, is a risk factor for type 2 diabetes, the metabolic syndrome, cardiovascular disease, and all-cause mortality. Recently, it was suggested that reducing sedentary time alone, regardless of the amount of time spent exercising, may be sufficient to improve glucose homeostasis in type 2 diabetes. Specifically, human intervention studies have demonstrated beneficial effects on postprandial plasma glucose and insulin levels when sedentary time is replaced with standing, walking, or brief bouts of exercise.
The goal of the study
Improvements in glucose control are evident following a four-day intervention in which two sitting replacement strategies were compared to a sedentary lifestyle. However, it is unknown whether such sitting-reduced regimens have a similar beneficial effect on insulin sensitivity and/or involve similar mechanistic pathways.
Remie et al. stated that the purpose of this study was to determine whether a sitting-less regimen (i.e. substituting low-level physical activities such as walking and standing for sedentary time) would be a viable and realistic alternative to exercise in the fight against insulin resistance. In insulin-resistant, obese postmenopausal women, they compared metabolomics and physiological responses to four days of acute exercise, sitting less, and/or sedentary behavior.
Methods
Remie et al. conducted a randomised three-arm crossover intervention study, with insulin sensitivity as the primary outcome measured using a two-step hyperinsulinaemic–euglycaemic clamp. Following 1H-MRS, muscle biopsy, and blood pressure measurements, a two-step hyperinsulinaemic–euglycaemic clamp was used to assess hepatic and peripheral insulin sensitivity. During the 1H-MRS measurement (at 07:00 a.m.), a primed, continuous D-6.6-[2H2]glucose (D2-glucose) tracer infusion (0.04 mg kg1 min1) was initiated. After three hours of D2-glucose pre-infusion, a three-hour primed low-dose continuous insulin infusion (10 mU m2 min1) was started to evaluate hepatic insulin sensitivity. Following that, a 2.5-hour priming high-dose continuous insulin infusion (40 mU m2 min1) was initiated to determine peripheral insulin sensitivity. Blood samples from arterialised blood were frequently taken to monitor the glucose levels required to maintain euglycaemia (5.0–5.5 mmol/l). During the last 30 min of the baseline, low and high insulin phases, steady state was reached, and blood samples were collected for determination of glucose tracer kinetics. Using indirect calorimetry, whole-body substrate utilization was also determined during these phases (Omnical; Maastricht Instruments, Maastricht, the Netherlands)
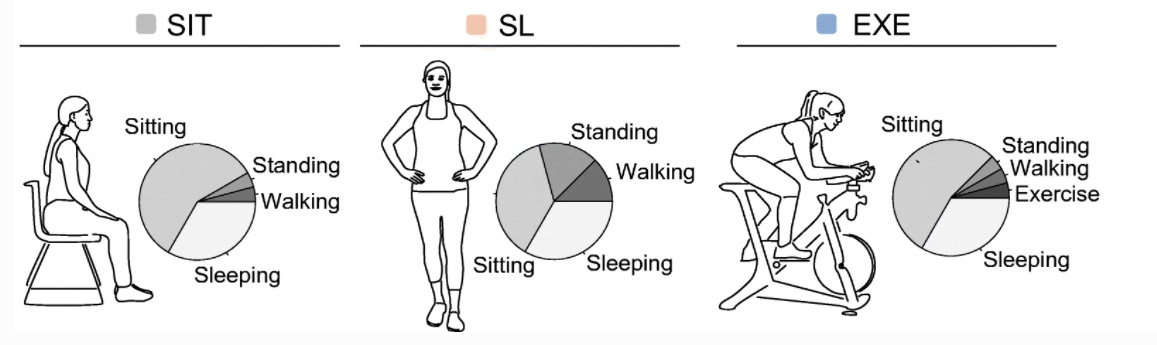
Fig. 1 Visualisation of the three activity regimens. Each participant followed the activity regimens in a random order.
Results
Remie et al. demonstrated that substituting light physical activities such as standing and walking for sedentary time improves peripheral insulin sensitivity. Exercise and a reduced-sitting regimen both had similar physiological effects on insulin sensitivity and underlying molecular metabolic changes in skeletal muscle, recapitulating certain aspects of the metabolic profile previously observed in athletes. This indicates that a sitting-reduced regimen may indeed alter the metabolome in a manner similar to that observed with exercise. Thus, sustained standing and walking may be a more appealing and possibly more feasible option for improving metabolic health than moderate-to-vigorous exercise.
How can we support your research?
Maastricht Instruments creates equipment in the field for indirect calorimetry and accelerometry. We provide support for Clinical research, E-health applications, accelerometry algorithms and data processing and analyses. Consult us about our accelerometry products, MOX1, MOX2, MOX3, MOX5 and BACE. or eHealth applications: Hospital Fit and Miss Activity
Reference
Remie, C.M.E., Janssens, G.E., Bilet, L. et al. Sitting less elicits metabolic responses similar to exercise and enhances insulin sensitivity in postmenopausal women. Diabetologia 64, 2817–2828 (2021). https://doi.org/10.1007/s00125-021-05558-5
https://link.springer.com/article/10.1007/s00125-021-05558-5
Related products:
Omnical RMR
The Omnical is the most versatile and accurate indirect calorimeter for research purposes on the market. Comprised of state-of-the-art technology using the highest-class precision measurement instruments, it enables customers to perform studies in various research fields. The system is designed to measure energy metabolism ranging from resting metabolism rate (RMR) to sports performance testing (e.g. VO2max tests) with high accuracy.
MOX1 Activity logger for physical activity assessment.
The MOX1 is a validated accelerometer-based activity logger that seamlessly measures and records high resolution raw acceleration data up to 7 days. By using the IDEEQ software featuring our proprietary algorithms, objective measurements of human physical activity can be classified and quantified. The waterproof system design and biocompatible adhesive ensures easy application and comfortable wear by the subject.
